
Living Up
Lessons to level up your life
Explore the intriguing potential link between food allergies and diabetes, dissecting immune response, diet impact, and current research.

Lately, an intriguing question has been making rounds in both scientific and casual circles, I can’t say I speak from experience because growing up I didn’t hear a lot about allergies, our family didn’t suffer from it and if they did, they never said anything about it, simply avoided certain foods. My current family does not suffer from it either, or at least not in the way other families do. Within the topic of health and well-being, the connection between our diets and overall health is undeniable. Whether it’s for maintaining an optimal weight or preventing various diseases, the food we consume significantly impacts our body’s functioning.
But, how can you relate what we eat to our body functions in relation to allergies when my nieces have suffered from them since birth. Other members of my family have suffered of diabetes and heart conditions, but the actions they take vary and so do the results, in that train of thought, can food allergies lead to diabetes? To tackle this proposition, I need to research and understand what we mean by food allergies.

Allergies, in their most general essence, are the body’s hypersensitive reaction to substances that are usually harmless. These reactions occur when our immune system misinterprets benign elements as threats and responds by launching a defensive attack. This results in various symptoms that we familiarize with an allergic reaction.
Maintaining a healthy diet is vital for everyone but even more so for people dealing with both food allergies and diabetes simultaneously since certain foods could potentially trigger adverse reactions while others may interfere with blood sugar management and insulin responses. It takes careful balancing as they navigate daily meals but understanding the nature of their condition is half the battle won.
Now let’s zoom into food allergies, a significant subset of allergies overall. Living with food allergies means having to be acutely aware of what you’re eating every day.
Food allergies occur when the immune system identifies proteins present in food as harmful intruders, which leads to the production of Immunoglobulin E (IgE) antibodies aimed at neutralizing these perceived threats. The subsequent interactions between these antibodies and proteins trigger the release of chemicals like histamine resulting in symptoms such as hives, difficulty breathing, or an upset stomach.
What’s important to remember is that allergens can vary from person to person. Some might have a severe reaction to peanuts while others might react adversely to shellfish or milk products; it’s all about your unique biology and how your immune system has been ‘programmed’ so far.

Food-related allergic reactions can cause inflammation which doesn’t just affect areas of direct contact like your mouth and stomach. This inflammation from food allergies could spread throughout your body via your bloodstream causing wider systemic effects like skin rashes or even respiratory difficulties.
The adverse reactions of allergies from food to certain foods range in symptoms from mild itching or rashes, to severe responses like difficulty breathing and even potentially life-threatening anaphylaxis. It primarily involves our immune system misidentifying some proteins in specific foods as harmful invaders, leading to inflammation from food allergies.
Now, food allergies: they’re quite the enigma and can significantly affect a person’s life. Imagine having an adverse reaction to something as simple and essential as eating! The culprits can range from dairy products to nuts, seafood to soy – everyday items that most of us enjoy without batting an eyelid.
What happens is basically your immune system overreacts to specific proteins in these foods because it mistakenly perceives them as harmful invaders. The resultant inflammation can manifest as hives or skin rashes, swelling, nausea or even life-threatening anaphylaxis. But let’s not forget about environmental allergies which are equally prevalent.
Food allergies are often the first that come to mind, but there’s a whole host of other types out there.
Anaphylaxis is an allergic reaction that can be fatal if not treated with the immediate medical attention it requires. According to the Mayo Clinic, “Anaphylaxis is a severe, life-threatening allergic reaction. It can happen seconds or minutes after you’ve been exposed to something you’re allergic to.” (Mayo, n.d.) The Mayo Clinic adds that some of the common symptoms may include:
Although our focus is on food allergies, we’ll briefly explore this pretty broad category. Allergies come in many shapes and forms, affecting people in different ways and to varying degrees. They are triggered by substances found in our surroundings like pollen, dust mites or animal dander – those pesky little particles shed by pets – causing symptoms like sneezing, watery eyes or itching.
Alongside food and environmental allergies we have drug allergies (reactions to certain medications), skin contact allergies (response to direct contact with allergens like latex), insect sting allergies (yes – reactions to insect venom) among others. Whew! It’s practically a minefield out there!
And here comes the kicker – how these disconcerting immune system responses might connect with conditions such as diabetes remains a topic of ongoing research. The aspect of inflammation from food allergies could potentially have implications for blood sugar regulation—further underscoring the importance of maintaining a healthy diet whether you’re dealing with food allergies or diabetes.
Essentially this vast world called ‘allergies’ is just one piece of the larger puzzle we’re trying to solve when it comes to understanding health conditions such as allergies and diabetes. Keep in mind though, everyone’s experience with both these conditions varies greatly – so it’s always paramount to consult with a healthcare professional for personalized advice.
Food allergies are a curious thing, they can sneak up on you at any age, turning your favorite snack into a dangerous foe. It’s not just about getting an itchy mouth or hives anymore; the reactions can be severe. Learn to recognize their symptoms, which can range from mild to life-threatening.
They often appear within minutes to several hours after eating the offending food. Now, although potential allergens are many and varied, there are some usual suspects that take the top spots.
These include foods like peanuts, tree nuts (like walnuts and cashews), shellfish, fish, milk, eggs and wheat. You might experience itching or swelling in your mouth or throat after consuming these foods if you’re allergic to them. More significant reactions might involve skin reactions such as hives or eczema flare-ups. But that’s not all!
Some people experience gastrointestinal issues like abdominal pains or diarrhea. In more serious cases – though luckily quite rare – there could be anaphylaxis: a potentially fatal allergic reaction causing difficulty breathing and shock.
So how does one know for sure if it’s a food allergy causing these symptoms? That’s where diagnosis comes in!
By understanding food allergies, we can consider the role inflammation from food allergies may play in the link with diabetes.
 Delving deeper into this fascinating connection between allergies and diabetes reveals how shared pathways within our intricate immune system might be at play here. In essence, both conditions – one causing adverse reactions to specific foods while another causing blood sugar imbalances – arise due to abnormal functioning of our immune responses.Despite ongoing research studying these linkages between food allergies and diabetes risks, clear-cut evidence establishing causality remains elusive. Interestingly though, some studies suggest potential indirect connections due to overlapping elements like inflammation or gut health disruption.
Delving deeper into this fascinating connection between allergies and diabetes reveals how shared pathways within our intricate immune system might be at play here. In essence, both conditions – one causing adverse reactions to specific foods while another causing blood sugar imbalances – arise due to abnormal functioning of our immune responses.Despite ongoing research studying these linkages between food allergies and diabetes risks, clear-cut evidence establishing causality remains elusive. Interestingly though, some studies suggest potential indirect connections due to overlapping elements like inflammation or gut health disruption.
The intricacies of the immune system are quite fascinating, and indeed, it plays a crucial role in tying together the concepts of allergies and diabetes.
When dealing with these two conditions concurrently, your healthcare team will likely follow certain diagnostic protocols closely related to the immune response at play. For instance, they might look at levels of immunoglobulin E (IgE), an antibody that becomes elevated during an allergic response.
Considering allergy as a form of autoimmunity brings us closer to understanding its potential link to diabetes. There’s also emerging interest in how food allergies may indirectly lead to diabetes through inflammation. An unhealthy diet high in allergenic foods can trigger chronic inflammation that throws off internal systems including metabolism and insulin regulation.
The hypothesis that allergies could lead to diabetes isn’t new; researchers have been exploring this theory for years. However, most current studies conclude there isn’t enough direct evidence yet to draw a definitive connection between generalized food allergies and developing diabetes.
It’s important though not to overlook the role of lifestyle habits, a healthy diet loaded with diverse nutrients boosts your gut health significantly and strengthens those good bacteria, which aid in metabolism regulation – making them a powerful ally against both inflammation from food allergies as well as blood sugar dysregulation associated with diabetes.
Autoimmunity is when our immune system gets a little confused and begins to see our own cells as foreign invaders. It then wages a war against our body, sadly turning out to be a self-destructive process.
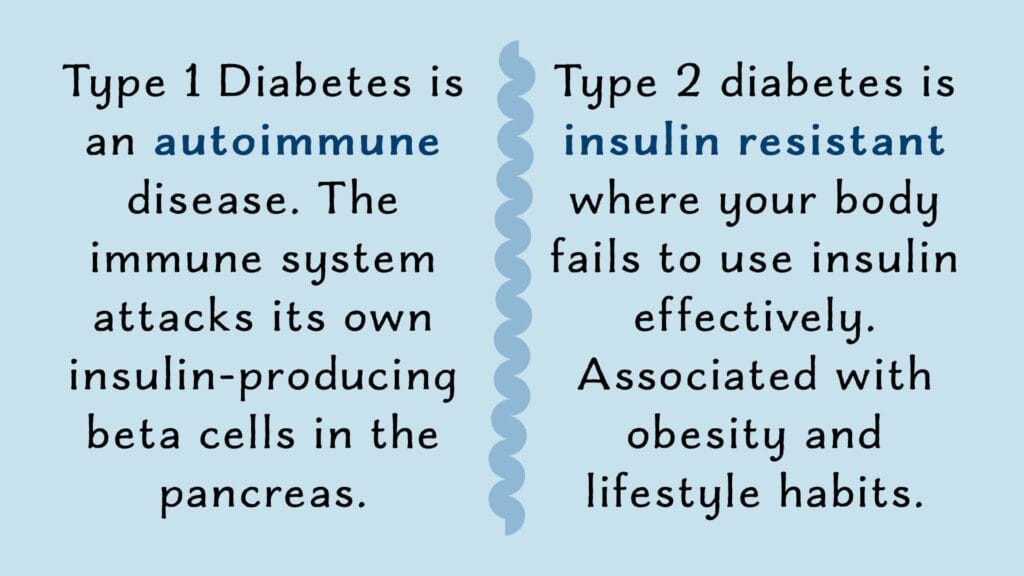
Type 1 diabetes is itself an autoimmune disease where the immune system destroys the insulin-producing beta cells in the pancreas. Interestingly enough, food allergies are also a result of immune confusion but in a slightly different way. Herein, innocuous food proteins are mistaken for harmful pathogens and an allergic reaction ensues. The connection comes into play because both situations involve an overactive or misguided immune response.
What’s more intriguing is that inflammation from food allergies could potentially contribute to insulin resistance, which is a key player in type 2 diabetes. It’s like your body is constantly on high alert due to these allergic reactions causing inflammation, which could lead to other health problems down the line if not managed properly.
Prevention is always better than cure, and maintaining proper nutrition is one of your best defenses against both, allergies and diabetes!
Scientists, researchers, and medical professionals are in continuous pursuit of understanding the complexities of our bodies. One intriguing proposition they’re currently examining is the hypothesis linking allergies, particularly food allergies, to diabetes. The immune response triggered by food allergies can potentially lead to a cascade of responses that could affect insulin production or use.
allergic response to a certain type of food is perceived by the body as a foreign invader and initiates an immune reaction which can trigger inflammation – it’s the body’s natural protective response in action. However, when inflammation becomes chronic due to regular exposure to allergens in your diet, it might potentially lead to insulin resistance.
That said, we must remember that this is just one hypothesis among many as numerous factors contribute towards developing diabetes such as genetics, lifestyle choices, and environmental factors.
It should also be noted that further research needs to be done in this area before any definitive conclusions can be drawn. While we wait for science to unravel this knot, maintaining a healthy diet that avoids known allergens could help manage, both allergies and diabetes, effectively.
Some scientists hypothesize that chronic inflammation, which is commonly observed in individuals with food allergies, might pave the way for insulin resistance over time, a key factor contributing to type 2 diabetes. a study where researchers are trying to map out this link more concretely explores how food allergies trigger an immune response in our bodies and whether this response has any long-term effects on our metabolic health. Their work is crucial not only to establish this possible connection, but also to determine if maintaining a healthy diet can help manage both conditions simultaneously.
The relationship between allergies and diabetes remains complex and somewhat elusive. It’s like trying to solve a puzzle with several missing pieces. every new piece of research adds another piece to this puzzle. By understanding these potential connections better, we can refine our dietary habits towards a healthier life — tackling allergic symptoms head-on!
Most scientific literature currently shows no direct link between food allergies and diabetes, yet even in the absence of concrete proof linking these two conditions, many professionals agree on maintaining a healthy diet toward managing both diseases effectively.
If you have food allergies and suffer from frequent bouts of inflammation due to allergies, eat anti-inflammatory foods such as fruits and vegetables to help improve your health overall. In essence then, while we may not currently have definitive answers about the connection between allergies and diabetes – we are reminded about focusing on overall wellness through balanced nutrition for optimal health.

We’ve explored the complex dynamics between allergies and diabetes, particularly food allergies. Amongst prevailing uncertainties and evolving research, there have been intriguing intersections exposed in immunology that hint at a link between these conditions. In our journey, we’ve found diabetes and allergies share common threads and crossroads.
Food allergy attacks are instigated by an over-zealous immune system that misidentifies harmless food proteins as threatening invaders, triggering an immune response targeting and destroying insulin-producing cells in the pancreas, which could have implications in developing Type 1 Diabetes.
Inflammation from food allergies is another significant concern. It can impact the gut health, disrupt metabolism and ultimately pave a pathway towards insulin resistance and Type 2 diabetes. Inflammation from food allergies might indirectly influence diabetes onset or management.
Maintaining a healthy diet that suits individual dietary restrictions due to allergens can help manage both conditions better. Focusing on gut-friendly foods can improve metabolism while keeping blood sugar levels stable even if you’re dealing with the dual challenge of managing diabetes amidst food allergies.
These hypotheses remain in need of solid backing. There is a shortage of direct scientific evidence confirming a definitive causation between food allergies and diabetes. Further comprehensive research is needed to understand this relationship fully.
Meanwhile adopting proactive strategies like a healthy diet, can help manage these conditions and potentially mitigate their progression or onset. For diabetics with food allergies, meal planning is essential. It’s about finding alternatives, maintaining adequate nutrient intake and avoiding foods that trigger allergies. It may demand an acute monitoring of diet, along with medications or insulin therapy for diabetes management, but you’re worthy.
To wrap up our research has made it abundantly clear that our gut health is directly linked to our overall well-being, further emphasizing the need to manage inflammation effectively. Stay informed and communicate often with your healthcare provider to better manage your health. One cannot stress enough the importance of a healthy diet in managing both these conditions.
Insulin is not a cure for diabetes; it is a treatment. It enables the diabetic to burn sufficient carbohydrates so that proteins and fats may be added to the diet in sufficient quantities to provide energy for the economic burdens of life.
– Frederick Bantig
Sources:
Frederick Bantig quote thanks to BrainyQuote.com
The Mayo Clinic. (n.d.). Anaphylaxis, Symptoms and Causes.





